What are Faecal Microbiota Transplants?
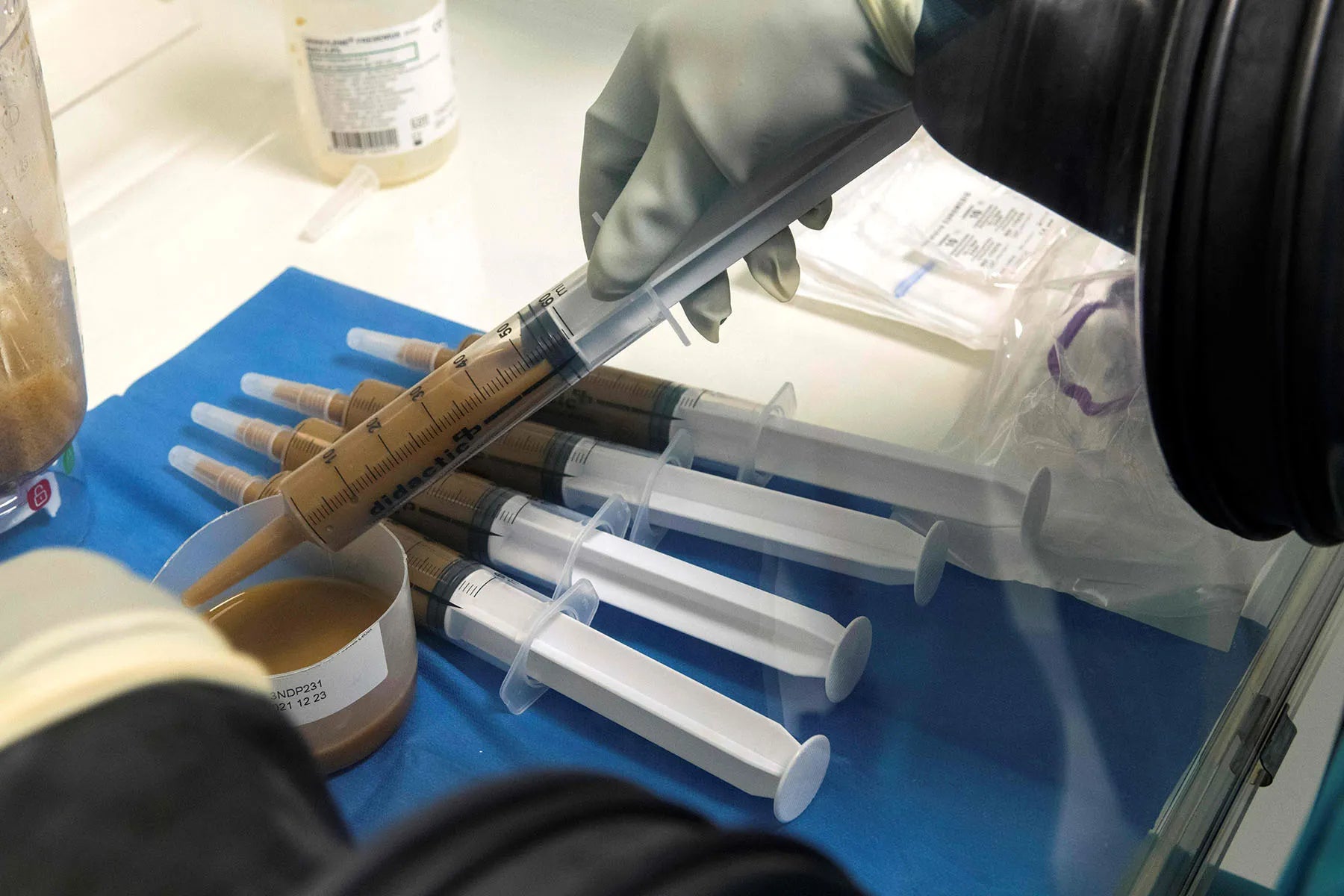
Faecal Microbial Transplants (FMT) sees normal ‘healthy’ human flora introduced into the patients bowel to ‘kill’ the bad bacteria and re-establish a microbiome full of 'good' bacteria. The infusion is repeated for at least 5 days or longer.
The high success rate and safety in the short term reported for recurrent Clostridium difficile infection has elevated FMT as an emerging treatment for a wide range of disorders, including Parkinson’s disease, fibromyalgia, chronic fatigue syndrome, myoclonus dystopia, multiple sclerosis, obesity, insulin resistance, metabolic syndrome, and autism.¹
Poo is collected from a screened donor, processed, tested and administered by a TGA accredited gastroenterologist. Once delivered, the host ideally adopts the microbiome profile of the donor and therefore experiences a far lesser likelihood of symptom relapse.
Human faeces from healthy donors contain vast amounts of beneficial bacteria that confer systemic health benefits — Unlike probiotic supplements, this bacteria permanently colonises in the patient giving the newly introduced ‘good’ bacteria a better chance of re-establishing dominance.
FMTs foster a healthy microbiome more effectively than antibiotics, probiotics or nutrition alone. They target the root cause of your symptoms — an imbalanced microbiome — and give you the best chance of achieving total symptom remission.
Donor Screening
Individual stool donor samples are screened under TGA guidelines, with full screening for all viral and bacterial pathogens.
All donors are regularly screened with serology (blood) tests and stool tests. Stool samples from all potential donors must be screened and shown to not contain a list of specified microorganisms that impact the quality and safety of the stool.
Conditions FMTs Have Been Studied In
Landmark Clinical Studies in FMT
| Condition | Key Study | Journal & Year | Primary Finding |
|---|---|---|---|
| Clostridium difficile | van Nood et al. | N Engl J Med, 2013 | Study stopped early due to clear superiority of FMT; 81% of patients in the FMT group had resolution of symptoms vs. 31% in the vancomycin-only group. |
| Ulcerative Colitis | Paramsothy et al. | Lancet, 2017 | Multi-donor FMT induced clinical remission in 27% of patients vs. 8% with placebo (p=0.02), with endoscopic remission seen in 19% vs. 5%. |
| Irritable Bowel Syndrome (IBS) | El-Salhy et al. | Gut, 2020 | FMT resulted in a significantly higher response rate (77.8%) compared to placebo (23.3%) at 1-year follow-up, with sustained effects at 3 years. |
| Anti-Aging | Ghosh et al. | Nat Rev Gastroenterol Hepatol, 2022 | Review concluding that gut microbiome is a key factor in age-related health decline, with targeted microbial restoration showing promise for healthier aging. |
| Alopecia Areata | Rebello et al. | ACG Case Rep J, 2017 | Case report of a patient with alopecia universalis experiencing significant hair regrowth (from 0% to >50% scalp coverage) after FMT for C. difficile. |
| Alzheimer's Disease | Vinderola et al. | EBioMedicine, 2023 | RCT found no significant differences in primary cognitive endpoints, but noted FMT was safe and may modulate immune and microbial profiles. |
| Autism Spectrum Disorder (ASD) | Li et al. | Front Psychiatry, 2022 | RCT showing a higher GI symptom improvement rate in the FMT group (43.75%) compared to placebo (18.75%) and a significant reduction in CARS score. |
| Bipolar Disorder | Parker et al. | Bipolar Disord, 2022 | Case study reporting significant improvement, with the patient's MADRS score dropping from 31 (severe depression) to 7 (remission) post-FMT. |
| Cardio-Metabolic Syndrome | Yang et al. | Nutrients, 2023 | RCT where HOMA-IR (insulin resistance) was significantly reduced by -2.06 in the FMT group at 12 weeks, with no significant change in the placebo group. |
| Chronic Fatigue Syndrome | Borody & Nowak | ACNEM Journal, 2017 | A review discussing the role of gut dysbiosis in CFS and presenting case studies where patients experienced significant symptom resolution after FMT. |
| Crohn's Disease | Zhou et al. | Int J Colorectal Dis, 2023 | A meta-analysis showing a pooled clinical remission rate of 48.1% and a clinical response rate of 66.8% in Crohn's patients treated with FMT. |
| Diabetes (Type 2) | Wu et al. | Front Cell Infect Microbiol, 2023 | FMT plus Metformin led to a significantly greater reduction in HbA1c (-3.06%) compared to Metformin alone (-1.82%) after 12 weeks. |
| Non-Alcoholic Fatty Liver | Witjes et al. | Gastroenterology, 2021 | FMT from lean donors did not significantly reduce liver fat content (primary endpoint) but did improve secondary measures like intestinal permeability. |
| Fibromyalgia | Holster et al. | Ann Rheum Dis, 2023 | An open-label trial where 8 out of 10 patients had a clinically relevant response (≥30% pain reduction) at 12 weeks after FMT. |
| Hepatic Encephalopathy | Bajaj et al. | Gastroenterology, 2017 | FMT significantly reduced both the number of HE episodes (1 vs 5, p=0.04) and hospitalizations compared to standard of care. |
| Motor Neurone Disease (ALS) | Mandrioli et al. | Front Neurol, 2019 | Protocol for a clinical trial to test if FMT can modify disease progression by increasing the number and function of regulatory T-cells. |
| Multiple Sclerosis (MS) | Makkawi et al. | Front Neurol, 2022 | Case series where 4 out of 5 patients showed improvement in fatigue scores, and 2 patients had a significant decrease in their EDSS disability scores. |
| Obesity | Depommier et al. | Nat Med, 2019 | This study on Akkermansia (a key gut microbe) improved insulin sensitivity by 34.2% and reduced total cholesterol by 8.68% vs. placebo. |
| Parkinson's Disease | Xue et al. | Medicine (Baltimore), 2020 | RCT showing significant motor symptom improvement; PDSS scores in the FMT group increased by 10.3 points more than the control group at month 3. |
| Psoriatic Arthritis (PsA) | Kragsnaes et al. | Ann Rheum Dis, 2018 | The first RCT of FMT in PsA showed no significant difference in disease activity (ACR20 response: 33% FMT vs. 40% placebo), but the treatment was well-tolerated. |
How do I access the treatment as a patient or referring practitioner?
References
Fecal microbiota transplantation (FMT) is the infusion of liquid filtrate feces from a healthy donor into the gut of a recipient to cure a specific disease. A fecal suspension can be administered by nasogastric or nasoduodenal tube, colonoscope, enema, or capsule. The high success rate and safety in the short term reported for recurrent Clostridium difficile infection has elevated FMT as an emerging treatment for a wide range of disorders, including Parkinson's disease, fibromyalgia, chronic fatigue syndrome, myoclonus dystopia, multiple sclerosis, obesity, insulin resistance, metabolic syndrome, and autism. There are many unanswered questions regarding FMT, including donor selection and screening, standardized protocols, long-term safety, and regulatory issues. This article reviews the efficacy and safety of FMT used in treating a variety of diseases, methodology, criteria for donor selection and screening, and various concerns regarding FMT.
Fecal microbiota transplantation (FMT) has been utilized sporadically for over 50 years. In the past few years,Clostridium difficileinfection (CDI) epidemics in the USA and Europe have resulted in the increased use of FMT, given its high efficacy in eradicating CDI and associated symptoms. As more patients request treatment and more clinics incorporate FMT into their treatment repertoire, reports of applications outside of CDI are emerging, paving the way for the use of FMT in several idiopathic conditions. Interest in this therapy has largely been driven by new research into the gut microbiota, which is now beginning to be appreciated as a microbial human organ with important roles in immunity and energy metabolism. This new paradigm raises the possibility that many diseases result, at least partially, from microbiota-related dysfunction. This understanding invites the investigation of FMT for several disorders, including IBD, IBS, the metabolic syndrome, neurodevelopmental disorders, autoimmune diseases and allergic diseases, among others. The field of microbiota-related disorders is currently in its infancy; it certainly is an exciting time in the burgeoning science of FMT and we expect to see new and previously unexpected applications in the near future. Well-designed and well-executed randomized trials are now needed to further define these microbiota-related conditions.
